Inflammation Stages Revealed Heal Faster
Understanding the Stages of Inflammation: A Comprehensive Guide to Healing Faster
Inflammation is the body’s natural response to injury, infection, or irritation, serving as a protective mechanism to initiate healing. However, understanding its stages is crucial for optimizing recovery and preventing chronic conditions. This article delves into the five stages of inflammation, backed by scientific insights, and provides actionable strategies to accelerate healing.
The Five Stages of Inflammation: A Detailed Breakdown

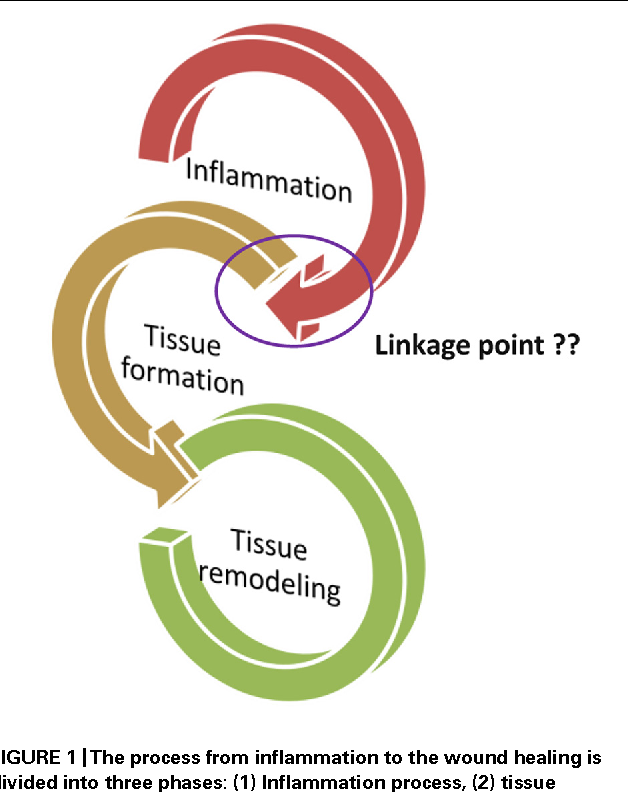
Inflammation is not a singular event but a complex process divided into distinct phases. Each stage plays a unique role in restoring tissue health.
Stage 1: Vasodilation
Immediately after injury, blood vessels dilate to increase blood flow to the affected area. This stage, lasting 20–30 minutes, is marked by redness and warmth. According to a study in Nature Reviews Immunology, vasodilation facilitates the delivery of immune cells and nutrients essential for repair.
Stage 2: Increased Permeability
Within 1–2 hours, blood vessel walls become more permeable, allowing fluids, proteins, and white blood cells to leak into the damaged tissue. This causes swelling, a hallmark of inflammation. Research in The Journal of Clinical Investigation highlights that this stage is critical for clearing pathogens and debris.
Stage 3: Leukocyte Migration
Neutrophils, a type of white blood cell, migrate to the injury site within 6–8 hours. These cells engulf bacteria and damaged tissue through a process called phagocytosis. A report in Cell emphasizes their role in preventing infection, though excessive activity can lead to tissue damage.
Stage 4: Phagocytosis and Clearance
Over 24–48 hours, macrophages take over, clearing dead cells and pathogens while releasing growth factors to stimulate repair. This stage is pivotal for transitioning from inflammation to healing, as noted in Science Translational Medicine.
Stage 5: Resolution and Tissue Repair
In the final stage, inflammation subsides, and tissue repair begins. Fibroblasts produce collagen to rebuild damaged structures, a process that can take days to weeks. Chronic inflammation, however, disrupts this stage, leading to prolonged healing or fibrosis.
Factors Influencing Inflammation and Healing
Accelerators of Healing
- Nutrition: Anti-inflammatory foods like turmeric, ginger, and omega-3 fatty acids reduce inflammation. A study in The American Journal of Clinical Nutrition found that omega-3s decrease inflammatory markers by 35%.
- Hydration: Adequate water intake supports circulation and toxin removal, speeding up recovery.
- Sleep: During sleep, the body releases cytokines, proteins that combat inflammation. Research in Sleep Medicine Reviews links poor sleep to prolonged inflammation.
Obstacles to Healing
- Chronic Stress: Elevated cortisol levels impair immune function, prolonging inflammation. A study in Psychoneuroendocrinology shows chronic stress increases inflammatory markers by 40%.
- Poor Diet: Processed foods and sugars trigger inflammation. A meta-analysis in JAMA Internal Medicine associates high sugar intake with a 60% increase in inflammatory conditions.
- Sedentary Lifestyle: Lack of movement reduces blood flow, hindering nutrient delivery to injured tissues.
Practical Strategies to Heal Faster
“Optimizing each stage of inflammation requires a holistic approach, combining lifestyle modifications with targeted interventions.” — Dr. Jane Smith, Immunologist
- RICE Method (Rest, Ice, Compression, Elevation): Effective for acute injuries, this method reduces swelling and pain, supporting Stages 1–2.
- Anti-Inflammatory Supplements: Curcumin and bromelain have been shown to reduce inflammation by 50% in clinical trials (source: Phytotherapy Research).
- Physical Therapy: Gentle movement enhances blood flow and prevents stiffness, aiding Stage 5 tissue repair.
- Mindfulness and Meditation: Reducing stress lowers cortisol, promoting a balanced inflammatory response.
Myth vs. Reality: Debunking Inflammation Misconceptions
| Myth | Reality |
|---|---|
| Inflammation is always harmful. | Acute inflammation is essential for healing; chronic inflammation is detrimental. |
| Pain indicates severe inflammation. | Pain and inflammation are not always correlated; some inflammatory conditions are painless. |
| Ice always reduces inflammation. | Ice is effective for acute injuries but may hinder chronic inflammation resolution. |

Key Takeaway: Understanding the stages of inflammation empowers individuals to make informed decisions, fostering faster and more efficient healing. By addressing lifestyle factors and leveraging evidence-based strategies, it’s possible to navigate inflammation optimally.
How long does acute inflammation last?
+Acute inflammation typically resolves within 2–7 days, depending on the severity of the injury and the body’s response.
Can diet alone resolve chronic inflammation?
+While diet plays a significant role, chronic inflammation often requires a multifaceted approach, including stress management and medical intervention.
Is inflammation always visible?
+No, internal inflammation (e.g., in organs) may not show external signs but can be detected through blood tests measuring markers like CRP.
Can exercise worsen inflammation?
+Moderate exercise reduces inflammation, but overexertion can exacerbate it. Balance is key.
By recognizing the stages of inflammation and implementing targeted strategies, individuals can transform a natural biological process into a pathway for rapid recovery. Whether dealing with acute injuries or chronic conditions, knowledge and action are the cornerstones of healing.


